
Reflections on Vancouver, British Columbia and other topics, related or not
Fixing fentanyl needs
investments in health and
housing to break deadly cycle
Vancouver’s mayor says his ride-along with ‘heroic’
first responders revealed the intensity of the problem
An opinion piece by Vancouver mayor Gregor Robertson, CBC News, February 2, 2017
Vancouver’s mayor says despite boasting North America’s first supervised injection sites
and having considerable community support, it still lacks the necessary, basic
health and housing supports to solve the overdose crisis. (Photo: CBC)
The fentanyl opioid crisis is a horrific public health emergency in Vancouver with an unprecedented overdose death toll. But solving it is possible with immediate and deliberate choices from all levels of government.
The latest numbers from 2016 show Vancouver had not only the highest number of deaths (215) but also the highest death rate from overdoses in B.C. This is staggering and heartbreaking — not least because every one of these overdose deaths was preventable.
There is no doubt we are in a tragic public health crisis, and we need all levels of government across Canada to treat it that way.
Our most vulnerable people
All corners of Vancouver are affected by the fentanyl opioid crisis, but it’s having a particularly devastating impact on our most vulnerable people.
Despite aggressively supporting harm reduction with North America’s first supervised injection sites and extensive education, research and peer support in the community, we lack the basic health and housing supports to solve the crisis.
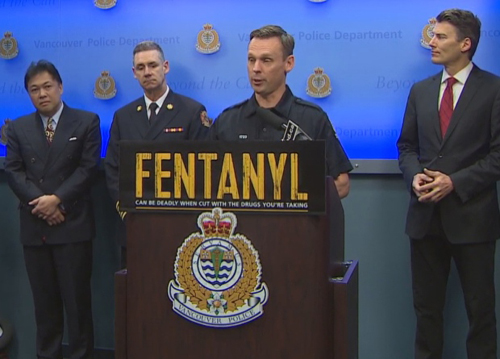
Mayor Gregor Robertson, second from right, prepares to speak on the ongoing overdose crisis
at VPD headquarters. Robertson says resources for front line emergency responders
and community workers are so strained, they’re reaching the 'breaking point.’
(Photo: CBC)
Today, there are an estimated 1,300 people in Vancouver using illicit opioids daily and not getting health care.
Users need treatment options that are immediate and accessible. Significantly improved access to opioid replacement therapy (Suboxone, methadone, prescription injectable heroin or hydromorphone) is urgently needed to help people break the cycle of addiction.
Currently, Crosstown Clinic is the only facility that offers a prescription heroin treatment program and it is overwhelmed with demand.
First responders under strain
Without adequate treatment, drug users can’t recover from their addictions and are relying on our first responders and front-line community workers to save their lives during overdoses.
Community groups and volunteers at pop-up sites have been heroic in their tireless efforts to save lives, but the intensity and frequency of these emergency calls is putting a severe strain on all our front-line workers.
It is overwhelming and not sustainable.
After a ride-along with firefighter medics at Fire Hall 2 in the heart of the Downtown Eastside last month, I saw first-hand just how true that is.
We know that people approach first responders and other service providers on a regular basis, seeking help for their addictions. However, treatment is not usually available, and when it is, gaps in the health system make it difficult to access.
One pop-up harm reduction site on the Downtown Eastside was averaging 110 supervised
injections a day. Gregor Robertson called the efforts of volunteers at these sites 'heroic’
but 'overwhelming and not sustainable.’ (Photo: Belle Puri)
Need to provide help immediately
When people come forward asking for health care, we need to provide them with that opportunity immediately for it to be effective. Breaking the cycle of addiction is critical to saving lives.
Other supports on the continuum of care are equally as vital to break this deadly cycle.
I’ve been fiercely advocating for more supportive housing and "housing first" programs with health supports, to give homeless drug users access to immediate housing and treatment options, with no requirement to abstain from drug use—a universal best practice recommended by the Mental Health Commission of Canada.
Investing in housing reduces other costs
Investing in housing has a ripple effect that reduces costs on our health care and justice systems. Federal and provincial support for health and affordable housing is at the crux of a broader, multi-faceted response needed to truly break the deadly fentanyl opioid death cycle.
Vancouver isn’t the only city to grapple with this crisis — major cities across Canada are ramping up to respond to the fentanyl opioid crisis.
I recently spoke with Prime Minister Trudeau about the overdose crisis and the importance of strong national leadership to ensure the resources, data and international best practices are coordinated across Canada.
A paramedic walks a woman into an ambulance on Vancouver’s Downtown Eastside
after firefighters had administered her a dose of naloxone. Gregor Robertson says
without more health care and housing supports, Vancouver’s most vulnerable
will continue to bear the brunt of the overdose crisis.
(Photo: Gian-Paolo Mendoza/CBC News)
The B.C. government is responsible for both health and housing, therefore has the most critical role ensuring that all people have access to evidence-based, effective treatment options and housing supports.
At a breaking point
The city continues to do more than its share to manage the fentanyl opioid crisis. We are intensifying our front line response, but we are at a breaking point: better access to addictions treatment, substitution therapy, detox and housing supports along the continuum of care is crucial to save lives and reduce the intense burden on everyone working to keep people alive and help them recover.
With hundreds of lives lost, it has never been more urgent to act.
Gregor Robertson is the mayor of Vancouver This story is part of CBC’s Opinion content. For more information, please read this editor’s blog and our FAQ.

.jpg)
